Frequently Asked Questions (FAQs)
What is an HSG, and why do I need it?
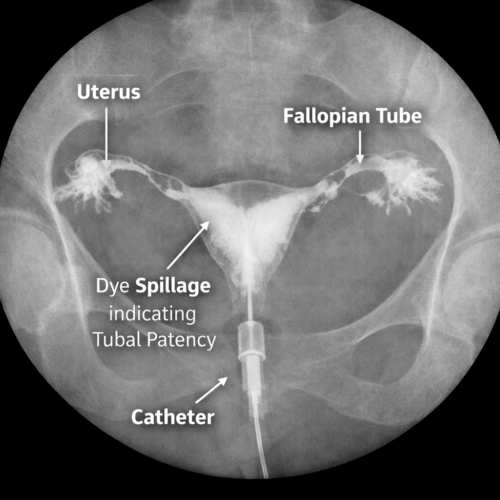
An HSG is an X-ray procedure used to evaluate the inside of the uterus and fallopian tubes to check for blockages or abnormalities. It’s often done in infertility workups to ensure the fallopian tubes are open for egg and sperm to meet.
Is the HSG procedure painful?
Some women experience cramping or discomfort similar to menstrual cramps during or after the procedure. The pain level varies from person to person.
How long does the HSG procedure take?
The procedure typically takes about 15 to 30 minutes. You may need to stay for observation afterward for a short period.
What should I expect after the HSG?
Some spotting and mild cramping are normal. Pain relievers can help manage discomfort. Most patients resume normal activities within a day.
Can the HSG improve my fertility?
In some cases, the dye used in the HSG can help flush minor blockages in the fallopian tubes, which might improve fertility.
When is the best time in my cycle to have the HSG?
The HSG is typically done after your period but before ovulation (days 7 to 10 of your cycle) to avoid the risk of performing the procedure during pregnancy.
Are there any risks associated with HSG?
Complications are rare but can include infection, allergic reactions to the dye, or very rarely, damage to the uterus or fallopian tubes.
What is an SSG, and why is it done?
An SSG is an ultrasound procedure used to assess the uterine cavity for abnormalities like polyps, fibroids, or adhesions. It involves injecting saline into the uterus for better imaging.
Is the SSG procedure painful?
Similar to the HSG, patients may experience mild cramping during the procedure, but it’s generally well-tolerated.
How long does the SSG procedure take?
The entire process usually takes 15 to 30 minutes.
What can I expect after the SSG?
Mild cramping or spotting is normal after the procedure, but these symptoms generally subside quickly. You can resume normal activities soon after.
Does the SSG affect my fertility?
The SSG is primarily a diagnostic tool, but identifying and treating any detected abnormalities can improve fertility.
When should I schedule the SSG?
Like HSG, SSG is done after menstruation but before ovulation (days 6 to 12 of your cycle) to avoid the risk of pregnancy.
Are there any risks with SSG?
Risks are minimal, but they may include mild infection or temporary discomfort. Serious complications are extremely rare.
How is SSG different from HSG?
SSG uses saline and ultrasound to evaluate the uterus, while HSG uses X-ray contrast dye to look at the fallopian tubes and uterus.
Both tests are important in diagnosing causes of infertility, and patients often ask about the differences, risks, and impact on their fertility.